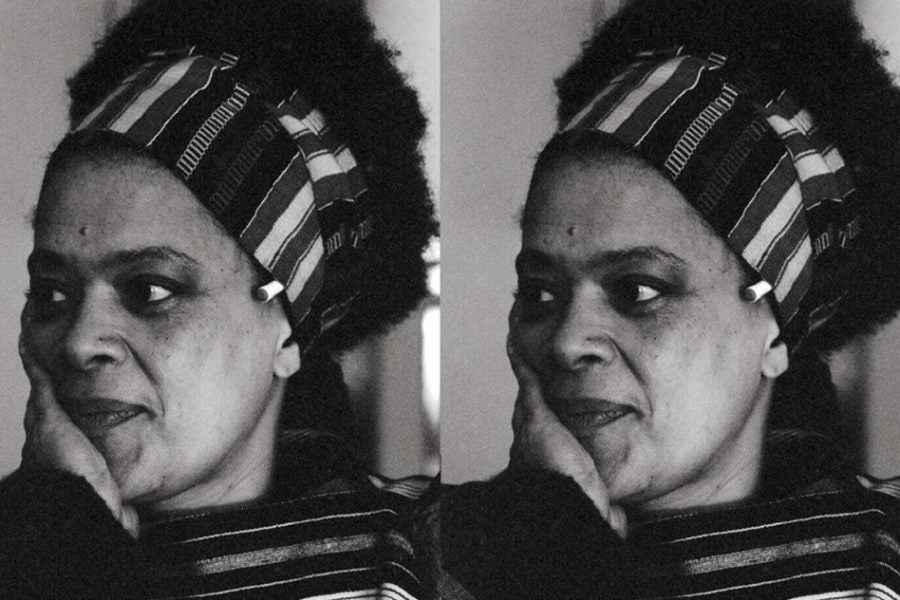
Thanks for reading Can We Talk?, a sex and relationships column that aims to tackle the burning questions about sex, dating, relationships, and breakups that you’re too afraid to ask your partner — or maybe even your besties. Last time, relationship therapist Moraya Seeger DeGeare, LMFT, helped a reader who couldn’t seem to find someone they wanted to date long-term. This week, she tackles a question from a reader with a question about navigating chronic pain and intimacy.
Do you have a dilemma or question you’d like to see answered as part of a future Can We Talk? Submit it here or send us an email at CanWeTalk@Refinery29.com
Dear Moraya,
I have migraines, endometriosis, and pelvic floor dysfunction. I’ve accepted that while I may not be in pain every day, pain will always be a major part of my life. I struggle to be honest about just how terrible this is, even with loved ones. This is impacting my relationships, especially romantic and sexual ones.
In order to have sex, I have to talk about my pelvic floor dysfunction, as I don’t currently have penetrative sex. While I feel fairly confident and secure in this, I still get stressed about telling new partners about it. My worry about their reactions (even when they’re positive) stops me from really being able to enjoy sex even after we have the conversation.
For example, I’d been dating a guy for a while and it felt like it was getting more serious. When I let him know what sex looks like for me, he didn’t say much in response, probably because he felt awkward and didn’t know what to say. While it wasn’t an enthusiastically supportive conversation, he believed me and didn’t ask me to do anything that would cause me pain (writing this, I’m realizing how horribly low my bar is for a “good reaction”). We had sex that night and I experienced lingering stress — I worried he’d ghosted me later (he didn’t). We kept talking, but I never felt I could open up to him about the other pain I was experiencing, as I felt I’d already overwhelmed him.
One other recent example: I took a first date home, which I don’t do often. After making out and cuddling for a while, I explained my situation. He was surprised and said he’d never heard of pelvic floor dysfunction. He ended up asking about what the condition is, how it works, why it happens, and how I handle it. It was honestly a much more supportive conversation than I’m used to having, and he seemed genuinely interested in understanding. We ultimately had sex, but I couldn’t get turned on enough to finish. I couldn’t figure out why, as our pre-hookup talk went so well. Since that first time, we’ve had sex a couple more times and I orgasmed.
But I want to know how to better open up about this with new partners and not let the pressure of doing so prevent me from enjoying sex. Honestly, I’m open to any tips for navigating conversations and hookups with potential new partners about chronic pain in general. I need help!
Sincerely,
Pain Point
Dear Pain Point,
Feeling physical pain can be excruciating. And you risk creating new pain — the emotional, heart-break kind — when you open up to anyone new, especially a romantic partner. But Pain Point, sometimes the latter form of pain is worth it.
I’ve navigated living with an autoimmune disease myself, and I have many people in my personal circles who deal with chronic pain daily. Many couples I support through therapy have dealt with trauma and pain, and we work on healing the disconnections that can occur in relationships due to these issues.
One thing I’ve picked up from my experiences: In order to get to the place you desire with future partners, it may require doing deeper work to get to a space of emotional safety and connection. This work starts within you. It sounds like you’ve already started it and come to a point of accepting your pain — but what about accepting and loving yourself?
You’ve already taken a great first step by just acknowledging the stress you’re feeling about being vulnerable with new partners, which is preventing you from feeling the way you want to during intimacy. This feeling is understandable. As any nervousness or anxiety increases, you are both distracted and pulled away from pleasure and bonding. There could also be added worry that the body will continue to tighten from the tension you’re feeling.
But, first, remember “Pain is a human experience and is valid,” says Jaimee Arnoff, PhD, a certified pain reprocessing therapist and my private practice partner. The migraines, endometriosis, and pelvic floor dysfunction are not something you have control over; but you can certainly utilize the resources available to you to live life fully.
Feeling physical pain can be excruciating. And you risk creating new pain — the emotional, heart-break kind — when you open up to anyone new.
Moraya Seeger DeGeare, LMFT
To set yourself up for success as you begin conversations about your journey with pelvic floor dysfunction — and other forms of pain when you feel secure enough to do so — I suggest first creating an environment that feels safe for you. That could mean asking to go to your place instead of theirs, or something else. Do you prefer being in motion on a walk when opening up? Or do you want to be sitting facing each other with a cup of tea to ground you and opportunities for eye contact?
When we talk about chronic pain, it’s vital to acknowledge the trauma that comes with it, possibly from both the original event or cause of the pain — and from the active trauma on your nervous system that can come from persistent pain. With this in mind, doing everything externally in your control to make yourself feel comfortable is key.
Communicating about your pelvic floor pain should involve talking about more than what you “can’t” do. It’s about discussing the emotions that you have about it, along with an emphasis on what does feel good physically. A positive sexual experience listens to both partners’ needs and involves connection, give and take, and honors safety for everyone to relax and play. If you’re not 100% sure what feels good for you (it sounds like you already have an idea), I’d turn to your community for advice on what they’ve found works.
For example, The Pelvic Floor Project podcast speaks with experts on the condition and offers great tips, noting how important it is to customize your treatment so that it aligns with your own beliefs about your body and sexual desires. In one episode, Amanda Olson, a physical therapist and pelvic expert, recommends spending up to 30 minutes a day by yourself in a safe environment touching yourself from different angles while deep breathing. By helping your body train the muscles to relax with different kinds of light pressure, it can help you feel more comfortable when someone else is consensually connecting with your body — and it can help you communicate what you want and need more effectively.
Another tip: It sounds like you’re making orgasming the end goal, which is an incredibly common source of anxiety in the bedroom. It’s amazing how much pressure it can take off when you focus more on “feeling pleasure” in general than “finishing.”
To help with the stress or pain that is distracting you during intimacy, I encourage you to incorporate these or any other practices that help you move back into your body. Listen to whether you’re actively craving this person Are you are feeling turned on by them? Or are you are having sex to make someone happy, to keep them around, or because you feel like you should want to?
You may be resistant to this idea of “getting into your body” at first. Most who deal with chronic pain are constantly trying to redirect their thoughts from wandering to parts of the body that are in pain. And you may even worry there’s a risk of becoming more acutely aware of the amount of pain you are in. If you try it and the pain is unbearable, listen to that, but you may also find you can hold both pleasure and pain at the same time. Maybe you’re used to intentionally trying to escape your body, using everything from heating pads to medication to dissociation — whatever helps. Your mind has been trained to feel the sensations in your body less, not more. This is when the dance between your pain, sex, and intimacy gets tricky. You have competing needs, and this may require mental acrobatics. I would encourage you to slow down a bit when connecting physically and to practice some exercises on your own to help connect your mind and body back together and to ultimately focus on the goal of simply feeling safe.
One practice to try: Focus on parts of your body that feel good and breathe into those spots first, reminding yourself that you have safe places to connect to already. Test them solo during masturbation first, then later when connecting physically with someone else. Then, when you notice the pain, distraction, and anxiety go up, you will feel confident that you have a whole fanny pack of well-practiced skills you can use in a bind to bring you back to feeling safe in your body as you relax into getting to know someone else’s. I also recommend reading the book Freedom from Pain for exercises similar to this one.
Chronic pain can feel like you are living in this silent, chaotic war with your own body. The tendency to avoid letting someone new in to join that battle makes sense. Especially if you’re worried it could lead to more hurt.
But to experience true intimacy, you have to be open to more pain of the heart, as noted. That could mean being rejected or misunderstood (sometimes the latter feels worse, honestly). Dating is so unpredictable at times — just like chronic pain. This is something we must learn to live with.
Chronic pain can feel like you are living in this silent, chaotic war with your own body. The tendency to avoid letting someone new in to join that battle makes sense.
MOraya Seeger DeGeare, LMFT
I want to encourage you to think about discussing your pain as an act that can spark connection and deeper understanding. One key thing I’ve learned working with couples navigating chronic pain is that not talking about it can be one of the biggest problems. Holding things in can even worsen the pain. The body’s heightened stress may trigger chronic flares, migraines, and other issues — and ‘round and ‘round you go. Allowing yourself to lean into that pain, talk about it when it feels organic, and ask for what you need will give the other person the freedom and permission to open up also. This is a huge part of healthy intimacy, and it’s certainly not a burden. As Dr. Arnoff puts it, “If you don’t give new partners a chance to be there in times of pain, how will you know if you’ll be able to depend on them when you really need them in the future?”
As you get to know someone or even get into a long-term partnership (if that’s something you want), and you’re having trouble revealing the whole of your pain, I encourage you to have continuous conversations and push yourself to be as open as possible. I would try not to go into these talks thinking: “Let’s get this over with.” Instead, trust these chats may lead to stronger bonds. And know that bringing your pain up — just like bringing up any subject that carries a lot of emotion for you — is inherently brave. You’re a warrior.
Equally, your body needs many moments of safety and reassurance, since it so often sits in states of pain that tell it exactly the opposite. There’s no shame in that — only strength in accepting it.
One last note: before you have these big conversations, I’d make sure you’re starting them with someone worthy of your time. I say this only because you mentioned having a “low bar” yourself. Although it sounds like you have come to a place of acceptance with your pain, perhaps you’re too accepting of those you let into your life. Get clear on what kind of partnership you are looking for. Ideally, the people you’re engaging with will have the emotional capacity to understand your pain and a craving to continue to learn your body’s needs, as I’m sure you will take the time to do with them.
I’ll leave you with this: Your chronic pain is currently a part of who you are, so let it be a part of you fully. If you love and embrace you, others will too.
DeGeare is a licensed marriage and family therapist, who specializes in intimacy, LGBTQIA+ relationships, mixed-culture couples, and racial identity development. The advice in this column is to point you in a direction that encourages healing and creates safety for you in this world. It is not to replace the relationship with a licensed mental health professional who knows your personal history.
Like what you see? How about some more R29 goodness, right here?
I Can’t Seem To Get Into A Long-Term Relationship
Help! How Do I Get Out Of A Toxic Love Triangle?